Managing nurse fatigue is crucial not only for the well-being of nurses but also for the safety and quality of patient care. A joint responsibility exists between healthcare employers and registered nurses to reduce fatigue-related risks and foster a safe, healthy work environment. Addressing nurse fatigue is no longer optional—it's critical to creating a sustainable healthcare system.
The American Nurses Association (ANA) emphasizes that both nurses and employers must prioritize rest and sleep to maintain safety, performance, and overall well-being. This article explores five key reasons why implementing a robust nurse fatigue management strategy should be at the forefront of every healthcare facility's operations.
The Alarming Prevalence of Nurse Fatigue
Nurse fatigue is a widespread issue with serious consequences. Studies show that 80% of nurses report getting fewer than six hours of sleep before their shift, far below the 7-8 hours recommended for optimal performance. A startling 55% of nurses consistently feel fatigued during their work shift, leading to diminished alertness and a higher risk of errors.
For healthcare employers, these statistics underscore the need for proactive fatigue management for nurses. By providing education and resources to help nurses manage their sleep and rest, healthcare organizations can reduce the risk of fatigue-related accidents and errors, and improve overall patient care quality.
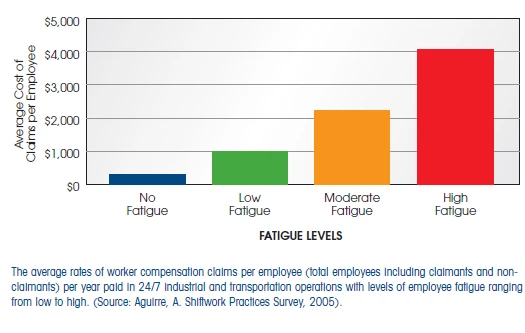
The healthcare sector reports the highest rates of workplace injuries compared to any other private industry. Fatigue plays a significant role in these statistics, with studies showing that fatigued workers incur up to four times the workers' compensation costs compared to well-rested employees.
The average workers' compensation claim for hospital injuries is $22,195, highlighting the financial burden associated with fatigue-related injuries. Managing nurse fatigue not only improves safety but can significantly reduce compensation claims, protecting both employees and the organization from the high costs of accidents.
The ongoing nursing shortage in the United States is a serious concern, with over 500,000 nurses expected to reach retireme by the end of 2024. The shortage of full-time registered nurses within the next two years is projected to be almost 80,000. High turnover rates—exacerbated by stress and fatigue make it challenging for healthcare facilities to maintain staffing levels.
Turnover rates are significantly higher in workplaces where fatigue is a pervasive issue. Replacing a single nurse costs between $27,000 and $103,000, depending on the region and specialty. Implementing a nurse fatigue management program can improve retention by reducing stress and fatigue-related burnout, offering a cost-effective solution to this growing problem.
Working long hours is often a necessity in healthcare, but research shows that excessive overtime leads to higher rates of workplace injuries. Nurses who work 12-hour shifts or more have a 37% higher injury rate, while those working over 60 hours per week see a 23% increased hazard rate. This is not just a concern for nurses but also impacts the patients they care for.
Managing nurse fatigue through optimized scheduling, proper rest periods, and limiting overtime can drastically improve nurse safety and reduce workplace injuries. A well-rested nurse is not only more efficient but also more capable of delivering safe, high-quality care.
The Joint Commission's Statement on Nurse Fatigue
Since 2011, the Joint Commission, which accredits over 20,000 U.S. healthcare organizations, has issued recommendations for healthcare facilities to implement a comprehensive fatigue risk management program. Their report, released in 2011 on Health Care Worker Fatigue and Patient Safety highlights the importance of mitigating fatigue to prevent adverse patient outcomes.
By creating and implementing a fatigue management plan, healthcare organizations can proactively address fatigue risks and uphold their commitment to providing safe, high-quality care. The Joint Commission's recommendations serve as a critical reminder of the need for structured approaches to managing nurse fatigue.
At the heart of every healthcare organization's mission is a commitment to excellence in patient care. However, this commitment cannot be fully realized without addressing the issues faced by the workforce—especially nurse fatigue. When nurses are fatigued, their ability to provide safe, effective care diminishes, leading to a ripple effect that can result in preventable errors and compromised patient safety.
Failing to manage nurse fatigue can ultimately undermine an organization's dedication to quality care, making it imperative for healthcare providers to prioritize fatigue management strategies.
Solutions for Managing Nurse Fatigue
Mitigating nurse fatigue requires a multifaceted approach that includes:
- Optimized Scheduling: Implement shift schedules that allow adequate rest between shifts, reducing the risk of burnout.
- Education and Training: Equip nurses with strategies to improve sleep quality and manage fatigue.
- Rest Policies: Ensure nurses have scheduled breaks and limit excessive overtime.
- Fatigue Monitoring: Use technology including a biomathematical fatigue risk model, and surveys to assess fatigue levels and intervene early when risks are identified.
By taking these steps, healthcare organizations can cultivate a safer, healthier work environment that benefits both nurses and patients.
Conclusion: Prioritize Nurse Fatigue Management for a Healthier Workforce
Addressing nurse fatigue is crucial for maintaining a safe, efficient healthcare environment. Fatigue management should be a core part of every healthcare facility's safety program, as it directly impacts patient care, nurse retention, and workplace safety.
To learn more about effective strategies for managing nurse fatigue, download our white paper, "Fatigued Nurses: Assessing the Risk, Implementing the Defenses," and discover how your organization can implement a successful nurse fatigue management program.
Ready to Optimize Nurse Fatigue Management?
Contact us today to explore how our expert solutions can help you develop a robust nurse fatigue management program, improve patient safety, and enhance overall nurse well-being and performance.
Interested in Shiftwork, Scheduling & Fatigue Risk Management Best Practices?
Subscribe to CIRCADIAN's email list for cutting-edge information, updated research findings, and easy-to-implement strategies, all tailored to optimize the health, safety, and performance of your shiftwork and extended hours operations.
Join our community of 32,000+ industry leaders and receive practical tips and expert insights to optimize your 24/7 workforce.